You might have heard frustration from a patient who has gone from doctor appointment to appointment with no change in diagnosis and feels unheard, ignored or dismissed OR, their symptoms/concerns have not been taken seriously. These are the first patients to seek out a new physician without first voicing their concerns and frustrations with their physician in order to gain a clear understanding of their protocols for diagnosis.
What you may not know is, healthcare providers must follow and provide evidence of conservative care; which takes time, patience, and multiple doctor visits to determine and support a diagnosis.
Our Observation:
Patients need patience and providers must clearly communicate their methods.
Before you seek out to find more attentive care, take time to talk with your physician… and keep in mind, that doctor hopping could cost you more time, and a lot more money.
New patients incur a bill based on the fee schedule for their 1st visit as well as any specific codes used to apply billing charges based on their appointment. They are determined not only by the type of provider you see, the classification of your visit, and the procedures provided, but fees are also applied for new patients at a different rate than returning patients.
While your medical records may follow you from doctor to doctor, the billing cycle as a new patient restarts every time you seek out a new healthcare provider.
Your Medical Billing Briefly Explained
As an outsourced billing solution, MEREM Healthcare Solutions delivers medical bills to patients and we also receive patient calls regarding those medical bills. Patients often request that we review and explain the charges that appear on the billing statement and the difference in costs on the EOB (explanation of benefits). Anytime your insurance has been filed, you should receive an EOB from your insurance company that explains
- What your insurance paid
- What was adjusted (contractual obligations)
- What the patient responsibility remains
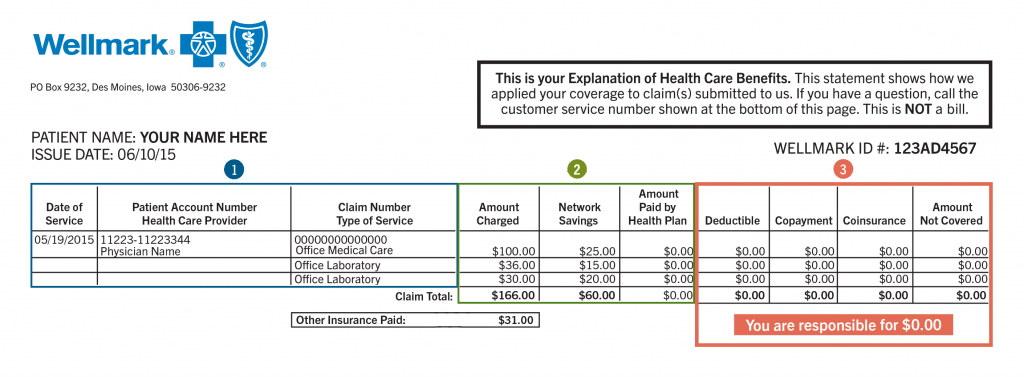
Image Source: https://www.wellmark.com/insurance-explained/your-benefits-in-action/how-to-read-your-eob
Looking at your EOB
For any consumer confused by the list of charges on your EOB and the possible difference in charges on your medical bill, you may not be fully aware of the contractual obligations between your provider and insurance company. Gaining a better understanding of a Fee Schedule and Contractual Obligation for yourself and from a provider perspective, may help.
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis. CMS develop fee schedules for physicians, ambulance services, clinical laboratory services, and durable medical equipment, prosthetics, orthotics, and supplies.
Contractual Obligation is the portion of the reimbursement from a payor that the provider cannot contractually expect payment for and cannot bill the patient for. It’s referred to as a “write-off” amount above the Allowed Amount or usual and customary rate.
For example, an office visit occurs and the provider bills the patient’s insurance or Medicare $100. The insurance company (or payor) has a set amount they’ve determined is appropriate compensation for that service. Maybe $60. The additional $40 charged to the payor is denied as Contractual Obligation with a remark code indicating that is the reason for denial. Then, depending on the policy, they (insurance company or Medicare) will pay all or part of the $60 and whatever portion is patient share will come out of that $60 as well. An 80/20 policy like Medicare would pay $48 and “deny” $12 as patient responsibility (coinsurance) and the provider would then bill $12 to the patient but NOT the additional $40 denied as Contractual Obligation.
Providers are subjected to fee schedules in order to regulate the cost of healthcare. The contractual obligations also known as adjustments, identify the difference in costs that providers are allowed to bill patients.
Our Observation:
Understanding financial responsibilities as a patient can relieve frustration and confusion after your office visit or procedure.
To avoid further frustration and confusion of your patient responsibility, there are 3 areas you as a consumer need to look for to better understand what your bill means.
- Deductible – patient responsibility owed before insurance will cover charges
- Co-insurance – the splitting of cost among insurance and patient (Usually 80/20 ratio of insurance covered, and patient cost owed after your deductible.)
- Co-payments – the sole patient responsibility that is due at the time of service
 The expert billing team at MEREM Healthcare Solutions is the primary point of contact for a patient’s statement and payment plan questions. Patients appreciate having their phone calls received directly by one of our U.S. based billing team members in our patient call center.
The expert billing team at MEREM Healthcare Solutions is the primary point of contact for a patient’s statement and payment plan questions. Patients appreciate having their phone calls received directly by one of our U.S. based billing team members in our patient call center.
