MACRA (Medicare Access and CHIP Reauthorization Act of 2015) is U.S. healthcare legislation that provides a new framework for how Medicare pays for physician services by incentivizing those who successfully demonstrate value over volume in patient care.
MACRA combines parts of the Physician Quality Reporting System (PQRS), Value-based Payment Modifier (VBM), and the Medicare Electronic Health Record (EHR) incentive program into one single program called the Merit-based Incentive Payment System, also known as MIPS.
In November, the Centers for Medicare and Medicaid Services (CMS) released their FINAL RULE for the 2019 Medicare Physician Fee Schedule. This Final Rule will go into effect January 1, 2019 for many clinicians and it is the start to the new physician payment provisions also known as the QPP. The CMS Quality Payment Program (QPP) has two tracks: the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs).
What is MIPS?
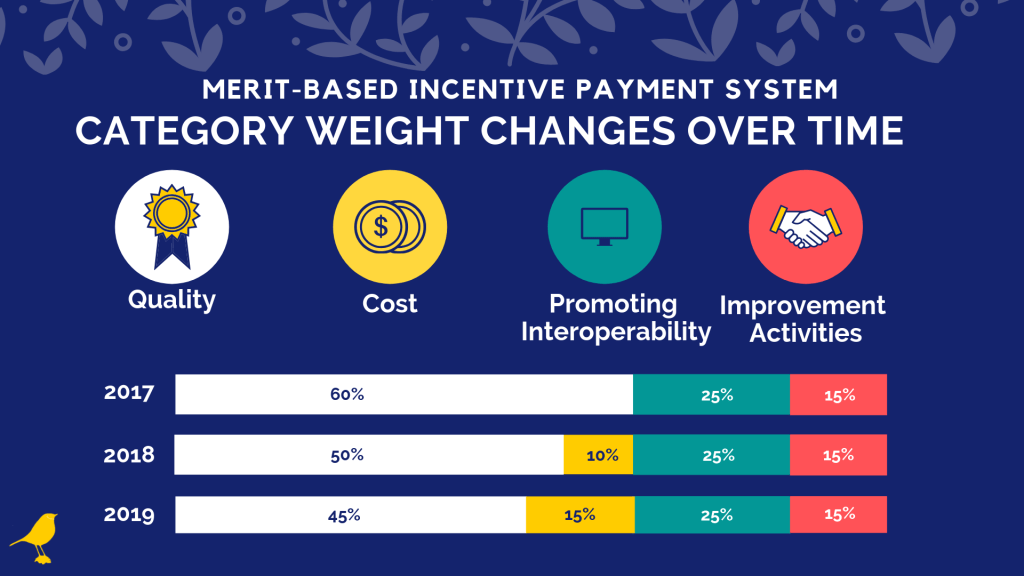
This is a healthcare law that doctors across the country, who accept Medicare patients, need to abide by in order to maintain or qualify for an increase in their reimbursement payments from the government. These physician incentives are based on clinical performance in four specific categories, Quality, Cost, Promoting Interoperability, and Improvement Activities.
These MIPS scoring weights have changed each year. The biggest changes in 2019 are
- Quality score reduced from 50% to 45%
- Cost score increased from 10% to 15%
- Improvement Activities: Interoperability bonus removed
- Eligible clinicians must use 2015 edition or newer certified EHR technology
- Performance Threshold minimum increased from 15 to 30 points. Exceptional Performance Range is at least 75 points.
For 2019, the Weights and MIPS final scoring rules, we found this webinar from Healthmonix to be extremely helpful.
In summary:
- Quality (45%) – Requires 6 measures to be reported with 1 outcome measure or high priority (specialty measure set)
- Cost Performance Reporting (15%) – based on 8 measures, 10 minimum procedural episodes such as knee arthroplasty, or 20 acute inpatient medical condition episodes
- Promoting Interoperability (25%) – Must report at least a 90 day period, Must use 2015 ed. or newer CERTEHR technology
- Clinical Practice Improvement Activities (15%) – 40 points required, based on weight.
If you are preparing for MIPS 2019 reporting, we hope this blog prepares your practice performance measures.
At MEREM Healthcare Solutions, we want to be your strategic partner in making sure your practice needs are met and your practice improvement and profitability are the end result. Contact us today to learn how our knowledgeable and experienced professionals can help assist or consult you with EMR technology and MIPS and MACRA submissions for your physicians.